Utilization management (UM) is one of those behind-the-scenes functions in healthcare that has a huge impact on patient care and payer operations.
Simply put, it’s all about making sure that the services provided to patients are necessary, effective, and in line with a payer’s policies.
But let’s be real; it’s no easy task.
Traditional UM workflows are a tangled web of manual steps. It starts with the intake of prior authorization requests, which can come in from all sorts of places: provider portals, email, and even fax. From there, the clinical documents have to be reviewed, checked against medical guidelines, and then sent back and forth between providers for clarification.
Oh, and let’s not forget about generating all the approvals and denials manually. It’s a lot of back-and-forth and takes up an enormous amount of time and effort.
The result?
Slow turnaround times, frustrated providers, and a heavy administrative burden that could be better spent elsewhere.
But what if this process didn’t have to be so complicated? What if automation could step in and make things faster, smoother, and more consistent?
Enter Power Automate, a game changer for streamlining UM workflows and making life easier for everyone involved.
In this article, we’ll explore how Power Automate can do just that, transforming UM workflows from a cumbersome process into a smooth, efficient operation.
Challenges in Traditional Utilization Management Processes
Despite its critical role in ensuring cost-effective and quality care, traditional utilization management (UM) processes often create significant operational and relationship challenges. These hurdles not only slow down workflows but also add friction between payers and providers, ultimately impacting patient outcomes.
Below are some of the most common pain points in the current UM landscape:
1. Long Turnaround Times for Prior Authorizations
Prior authorization remains one of the most time-consuming parts of UM. Because requests often rely on manual intake, data entry, and document review, processing can stretch across several days, or even weeks. Each additional step introduces delays that directly affect patient care, leaving providers unable to move forward with treatments or prescriptions until approval is secured.
For patients, this can mean postponed procedures, prolonged discomfort, and in some cases, worsening conditions. For payers, these delays create inefficiencies and bottlenecks that ripple throughout the entire care delivery system.
2. High Administrative Burden on UM Staff
Utilization management teams often juggle mountains of paperwork, repetitive data entry, and manual communication channels such as fax and email. Reviewing lengthy clinical documentation, cross-checking requirements, and responding to inquiries consume much of their time.
This administrative load leaves little room for higher-value work, such as improving UM protocols or addressing complex cases. Over time, the heavy workload contributes to staff fatigue, burnout, and high turnover rates, further straining payer organizations that are already stretched thin.
3. Inconsistencies in Decision-Making
Because manual review processes depend heavily on the individual staff member’s expertise, judgment, and interpretation, there is a high risk of inconsistency. Two reviewers might reach different conclusions when evaluating the same clinical information, which can frustrate providers and introduce compliance risks for payers.
These inconsistencies also undermine the standardization and transparency that providers expect, eroding trust and sometimes leading to disputes or appeals that further delay care.
4. Provider Dissatisfaction Due to Delayed Responses
Providers, under constant pressure to deliver timely, efficient patient care, are often forced to wait on prior authorization approvals before moving forward with treatment. Delays disrupt care plans, complicate scheduling, and place additional strain on provider-patient relationships.
When communication between payers and providers is slow or inconsistent, frustration mounts, leading to dissatisfaction on the provider’s side. Over time, this breakdown in collaboration can damage relationships between payers and providers, making it harder to maintain alignment on shared goals of quality care and patient satisfaction.
How Power Automate Transforms Payer Utilization Management
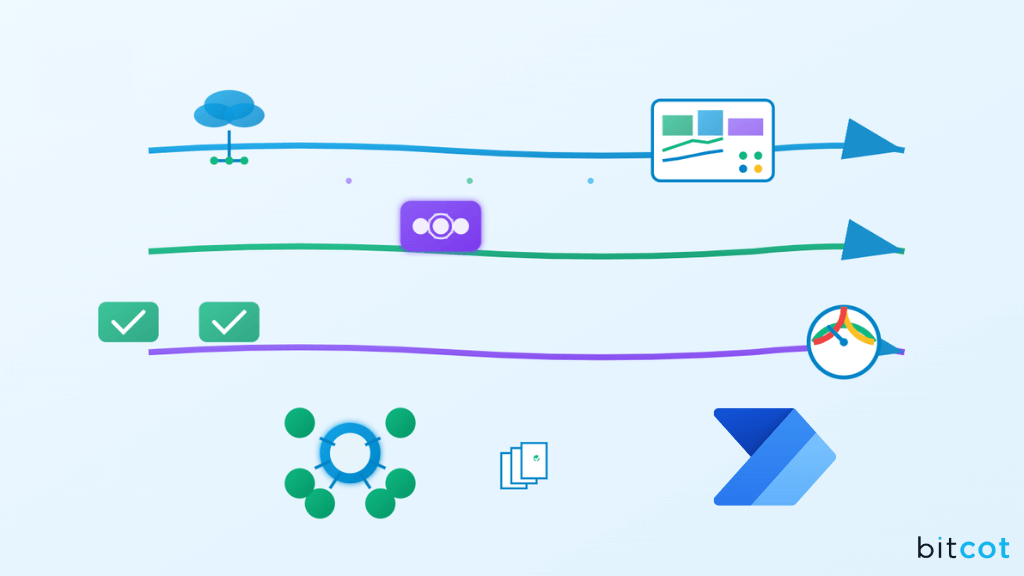
The good news is that Power Automate can take these manual, error-prone tasks and turn them into an efficient, automated utilization management process. By orchestrating workflows end-to-end, Power Automate can save time, reduce errors, and help your team focus on what really matters.
Here’s how it works:
1. Automating Intake of Authorization Requests
The first step in any UM process is capturing authorization requests, which can come from a variety of channels, whether it’s through a provider portal, email, or EHR system. Power Automate can automatically handle these inputs, ensuring that every request is captured as soon as it’s submitted. No more waiting for someone to manually check emails or log into systems.
2. Extracting and Validating Clinical Information
Once an authorization request is received, the next step is to extract the necessary clinical details. This typically involves a lot of manual data entry and document review, but with Power Automate, AI-powered tools like Form Processing can extract key data, such as patient ID, diagnosis, and service codes, directly from submitted documents.
The system can then validate whether the required information is complete, cross-checking against the patient’s records to ensure accuracy.
3. Running Compliance Checks Against Guidelines
Next, Power Automate can run automated checks to compare the request against established medical guidelines. By connecting to a policy database or even using AI models, Power Automate ensures that the request aligns with medical necessity rules. It can instantly flag non-compliant requests or any that need further review, reducing the chances of human error or inconsistent decision-making.
4. Routing Complex Cases for Medical Reviewer Approval
Some requests are more complex and require a clinical expert’s review. Instead of manually sorting through these cases, Power Automate can intelligently route them to the appropriate medical reviewer, whether that’s a nurse, medical director, or specialist.
It can even present the necessary information in an easy-to-read format, such as adaptive cards in Microsoft Teams, to help the reviewer make decisions quickly.
5. Generating Automated Correspondence Back to Providers
Once a decision is made, Power Automate can automatically generate and send the approval or denial letters to providers. Whether it’s populating a Microsoft Word template or converting documents to PDFs, the system can handle it all, without any manual effort. Correspondence is sent instantly, ensuring providers are updated in real-time and can take next steps accordingly.
6. Creating Audit Logs for Compliance
Last but not least, compliance is always top of mind in healthcare. With Power Automate, every step of the process, from intake to decision-making, is logged and documented automatically. These audit logs ensure that your organization stays compliant with healthcare regulations, and they’re easily accessible if you need to review or report on decisions.
How to Automate Payer Utilization Management with Power Automate
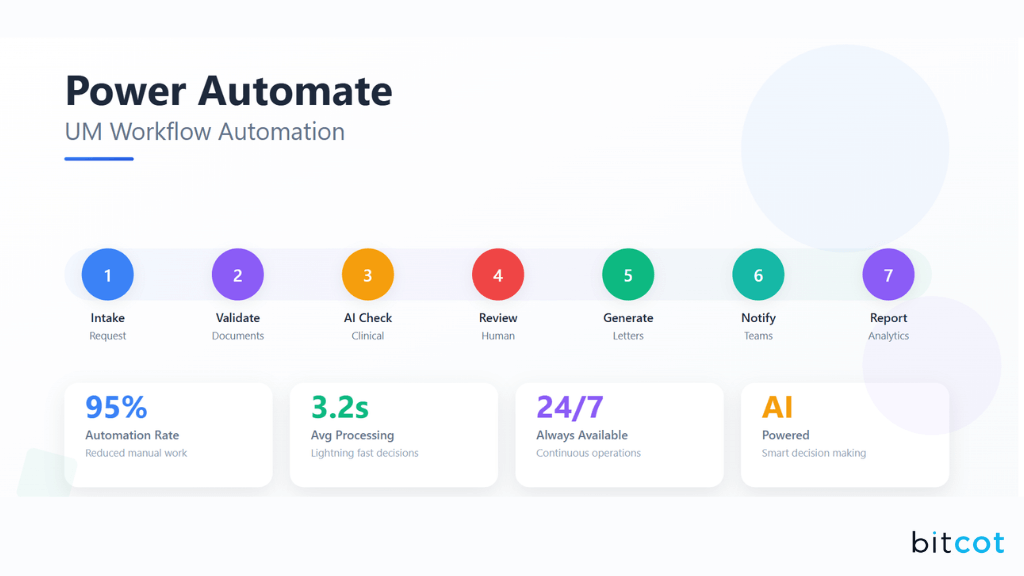
Automating the utilization management process with Power Automate can significantly improve efficiency and reduce manual tasks.
Here’s how to break down the entire process into easy-to-follow steps:
Step 1: Request Intake & Preprocessing
The first step is capturing and processing incoming authorization requests. These may come through various channels like provider portals, EHR systems, or even email. Power Automate ensures that every request is captured automatically and processed seamlessly.
Power Automate Actions:
- When a new response is submitted: Capture portal intake automatically.
- When a new email arrives (V3): Process emailed requests and extract attached clinical documents.
- Get file content: Retrieve clinical documents for further processing.
- Extract information from documents: Use AI Builder Form Processing to pull key data like patient ID, diagnosis, requested service, and provider details.
Step 2: Document Extraction & Validation
Once the authorization request is captured, the next step is to extract and validate the clinical data. It’s crucial to ensure that all required information is present and accurate before proceeding.
Power Automate Actions:
- Condition: Check if required fields (e.g., patient info, service code, provider ID) are available.
- HTTP: Query the EHR system to cross-check the patient’s eligibility.
- Send an email (V2): Notify the provider if any documents are incomplete or missing key information.
Step 3: Clinical & Compliance Checks
At this stage, Power Automate will run automated checks to determine whether the requested services meet clinical guidelines and medical necessity rules.
Power Automate Actions:
- Predict: Use AI Builder to assess whether the service request is in compliance with guidelines.
- SQL Server – Get rows: Pull policy or medical necessity rules from your database.
- Condition: Automatically flag requests as compliant or non-compliant, ensuring faster, consistent decision-making.
Step 4: Routing for Review (AI + Human-in-the-loop)
For more complex or unclear cases, Power Automate can intelligently route them to clinical reviewers for a human touch. This ensures that nuanced cases are handled with expertise, while still benefiting from automation.
Power Automate Actions:
- Start and wait for an approval: Automatically assign cases to a medical director or nurse reviewer.
- Post adaptive cards and wait for a response: Present the patient summary and guidelines in Teams to facilitate quick decision-making.
- Condition: Capture the reviewer’s decision (approval, denial, or request for more info).
Step 5: Decision & Correspondence Generation
Once a decision is made, Power Automate takes care of generating and sending approval or denial letters automatically, reducing administrative burden and improving response times.
Power Automate Actions:
- Populate a Microsoft Word template: Generate approval or denial letters based on the decision.
- Convert Word document to PDF: Convert the document into a final, shareable PDF.
- Send an email (V2): Send the letters to providers immediately.
- Update item: Record the decision in your UM system for tracking and reporting purposes.
Step 6: Notifications & Tracking
Keeping all stakeholders informed is crucial for a smooth process. Power Automate enables real-time notifications, ensuring everyone is updated on the status of requests.
Power Automate Actions:
- Post message in a chat or channel: Notify UM staff and provider relations teams about the status of requests.
- Send push notifications: Alert clinical reviewers about pending decisions or requests for additional information.
- Update item: Track the status of requests (e.g., Pending → Approved/Denied).
Step 7: Audit Logging & Reporting
Lastly, Power Automate ensures that every step of the process is documented and logged for compliance and performance tracking. This helps maintain regulatory standards and allows for better reporting.
Power Automate Actions:
- Add a row into a table: Log decision details and any relevant data into Excel or Dataverse.
- Convert file: Store letters and decision artifacts in PDF archives for future reference.
- Refresh a dataset: Update Power BI dashboards to provide insights into UM performance, such as turnaround times, denial rates, and compliance levels.
This step-by-step breakdown illustrates how Power Automate can simplify and streamline each stage of the payer utilization management process, from intake to compliance checks and final reporting.
By automating these tasks, healthcare payers can significantly improve efficiency, reduce errors, and enhance the overall provider experience.
Benefits of Automating Payer Utilization Management with Power Automate
Adopting automation in utilization management isn’t just about saving time; it’s about creating real, measurable improvements across the payer workflow.
With Power Automate, health plans can reimagine the way prior authorizations are handled, turning a traditionally slow, manual process into one that is faster, smarter, and more consistent.
Let’s dive into the key benefits in detail.
Faster Authorization Processing
One of the biggest frustrations in traditional UM is the time it takes to process requests. Staff have to sift through emails, download attachments, and manually enter information into systems before a decision can even be made. This often drags the process out for days, leaving providers and patients waiting.
Power Automate dramatically changes this dynamic. Requests coming in through provider portals, EHR integrations, or email can be automatically captured and routed. Clinical documents are read instantly using AI-powered extraction, and eligibility checks can run in the background without human intervention.
What once took multiple touchpoints and manual backlogs can now happen within hours. The result? Patients get timely care, providers experience fewer delays, and payers build trust by responding faster.
Consistency in Decisions
Manual reviews introduce human variability. Two staff members might interpret the same clinical guidelines differently, leading to inconsistent outcomes and confusion for providers.
With Power Automate, compliance checks can be standardized using AI Builder and database lookups. Every request is evaluated against the same rules, ensuring a fair and consistent process.
For more nuanced cases, automation can flag exceptions and escalate them to clinical reviewers, ensuring human expertise is applied only where needed. This approach not only reduces decision variability but also builds confidence among providers that decisions are being made objectively and consistently.
Reduced Administrative Burden
UM teams often spend the bulk of their time on repetitive, non-clinical tasks: downloading documents, entering data, checking eligibility, and drafting correspondence. These tasks are not only time-consuming but also mentally draining, leaving less energy for high-value work.
By automating these repetitive steps, Power Automate allows staff to shift their focus toward tasks that truly require clinical judgment or human empathy, like complex case reviews or provider outreach.
Instead of drowning in manual processes, staff become empowered problem-solvers and decision-support experts. This not only improves productivity but also boosts job satisfaction and reduces burnout.
Enhanced Provider Satisfaction
For providers, prior authorization delays can disrupt patient care and create unnecessary friction with payers. Waiting days for an approval, or chasing down missing documentation, leads to frustration and wasted time on both ends.
Automation shortens this cycle significantly. With faster intake, automated validation, and real-time notifications, providers receive timely updates and clear correspondence. Approval and denial letters can be generated and delivered almost instantly once a decision is made.
By reducing delays and improving communication, Power Automate helps strengthen payer-provider relationships, turning what was once a pain point into a smoother, more collaborative experience.
Compliance Assurance
Healthcare regulations require payers to maintain thorough documentation of every UM decision. In manual workflows, tracking every email, approval, and document can be overwhelming, and missing details create compliance risks.
Power Automate removes this concern by creating audit logs automatically. Every step, from request intake to reviewer approval to final correspondence, is captured and stored. These logs can be tied directly to reporting dashboards in Power BI, giving compliance teams and leadership full visibility into turnaround times, denial rates, and adherence to guidelines.
When audits come around, everything is already organized and ready for review, reducing risk and reinforcing payer accountability.
Future Enhancements in Utilization Management Automation for Payers
Power Automate already brings significant efficiency and consistency to utilization management, but the future holds even greater potential.
By layering AI, interoperability, and real-time engagement on top of Power Automate, payers can achieve not just efficiency, but also smarter decision-making and stronger provider relationships.
As healthcare payers look to further modernize their workflows, several enhancements can take automation to the next level:
Integration with FHIR APIs for Deeper EHR Interoperability
Today, much of the intake and validation process relies on connecting to multiple systems in fragmented ways. By integrating with FHIR (Fast Healthcare Interoperability Resources) APIs, payers can achieve seamless, real-time data exchange with provider EHRs.
This means patient eligibility checks, service history, and supporting documentation can be pulled instantly, reducing delays and minimizing manual verification.
NLP Models for Unstructured Clinical Document Understanding
Clinical records often come in unstructured formats like PDFs or free-text notes, making it difficult to extract meaningful information. With Natural Language Processing (NLP), Power Automate could interpret these documents just like a human reviewer, identifying diagnoses, procedures, and supporting evidence without manual input.
This enhancement would unlock a new level of efficiency by automating a traditionally time-intensive part of UM.
Chatbots for Real-Time Provider Communication
One of the biggest provider frustrations is not knowing the status of their authorization requests. By introducing chatbots, powered by Microsoft Teams or integrated portals, providers could check UM status in real time, ask follow-up questions, and even upload missing documents directly.
This would significantly reduce back-and-forth emails, while also improving transparency and provider satisfaction.
Predictive Analytics for High-Risk Request Flagging
Looking ahead, Power Automate can be combined with predictive analytics to identify high-risk or complex requests before they reach a reviewer.
For example, machine learning models could analyze historical data to predict which requests are more likely to require additional documentation, denial, or escalation. By flagging these upfront, payers can proactively route cases, allocate resources, and shorten resolution times.
Partner with Bitcot to Automate Payer Workflows with a Custom Solution
Choosing the right healthcare software development partner is critical when reimagining payer workflows.
At Bitcot, we go beyond off-the-shelf solutions by designing automation strategies that align with your organization’s unique needs, compliance requirements, and long-term goals.
Here’s why leading payers trust us:
- Deep Expertise in Healthcare Automation: Bitcot has extensive experience working with payer systems and understands the complexities of utilization management. Our solutions are built to integrate seamlessly with existing platforms while reducing friction for both staff and providers.
- Custom-Built Solutions, Not One-Size-Fits-All: Every payer has different policies, workflows, and regulatory challenges. We specialize in creating tailored healthcare software solutions that reflect your organization’s processes, delivering higher adoption rates and better outcomes.
- Focus on Compliance and Security: In healthcare, compliance is non-negotiable. Bitcot builds solutions with HIPAA and industry standards in mind, ensuring data privacy, audit readiness, and regulatory alignment at every step.
- Proven Ability to Reduce Turnaround Times: Our automation strategies are designed to accelerate prior authorizations and streamline communication, helping payers cut approval times significantly and deliver faster care decisions.
- Human + Technology Approach: We don’t just replace manual work; we enhance it. By automating repetitive tasks, UM staff gain more time to focus on critical, high-touch cases where human judgment is irreplaceable.
- End-to-End Support and Partnership: From discovery and design to implementation and scaling, we work closely with your teams to ensure solutions are adopted smoothly and deliver measurable ROI. Bitcot is not just a vendor; we act as your long-term partner in process transformation.
- Future-Ready Scalability: Our solutions are built with growth in mind, enabling you to expand automation capabilities as payer needs evolve, whether it’s integrating AI-driven decision support, analytics, or predictive insights in the future.
If you’re ready to reduce administrative burden, speed up authorizations, and deliver better provider experiences, our team can help you build the right Power Automate solution.
Final Thoughts
Utilization management has long been one of the most complex and resource-heavy functions for healthcare payers. Manual processes, inconsistent decisions, and provider frustration have made it a pain point for both payers and providers.
But with Power Automate, there’s now a clear path to simplify and modernize UM workflows.
By automating intake, validation, compliance checks, routing, correspondence, and audit logging, payers can transform UM into a faster, more consistent, and more transparent process.
The result? Shorter turnaround times, fewer errors, happier providers, and stronger compliance.
What’s even more exciting is that this is just the beginning. With future enhancements like FHIR integrations, NLP-powered document understanding, and predictive analytics, Power Automate has the potential to not only streamline UM but also make it smarter and more proactive.
At Bitcot, we empower payers to embrace this future with tailored workflow automation services that fit seamlessly into your existing systems.
Whether you’re looking to reduce costs, speed up approvals, or modernize provider interactions, we’ll help you design and implement a Power Automate solution built for long-term success.
Let’s talk about automating your UM workflows today.












